Managing billing and collections in a healthcare practice is no small task. It’s a delicate balancing act—ensuring claims are submitted accurately, payments are collected on time, and compliance with ever-changing regulations is maintained—all while focusing on providing the best possible care for your patients.
At Cadence Collaborative, we understand how overwhelming this can feel, and that’s why we’re here to help.
With our expertise in Outsourcing Medical Billing & Collections, we take the stress off your shoulders, simplifying your revenue cycle and giving you the freedom to focus on what truly matters: your patients.
This guide is designed to walk you through everything you need to know about outsourcing your billing and collections, from how it works to the benefits it can bring to your practice.
What Is Medical Billing Outsourcing?
Let’s start with a simple idea: your revenue cycle is the lifeline of your healthcare practice. It’s how you track everything, from the moment a patient schedules an appointment to the point when their bill is fully paid.
Managing this process can be overwhelming, especially when you add in the complexities of medical coding, insurance claims, and payment follow-ups. That’s where outsourcing medical billing comes into play.
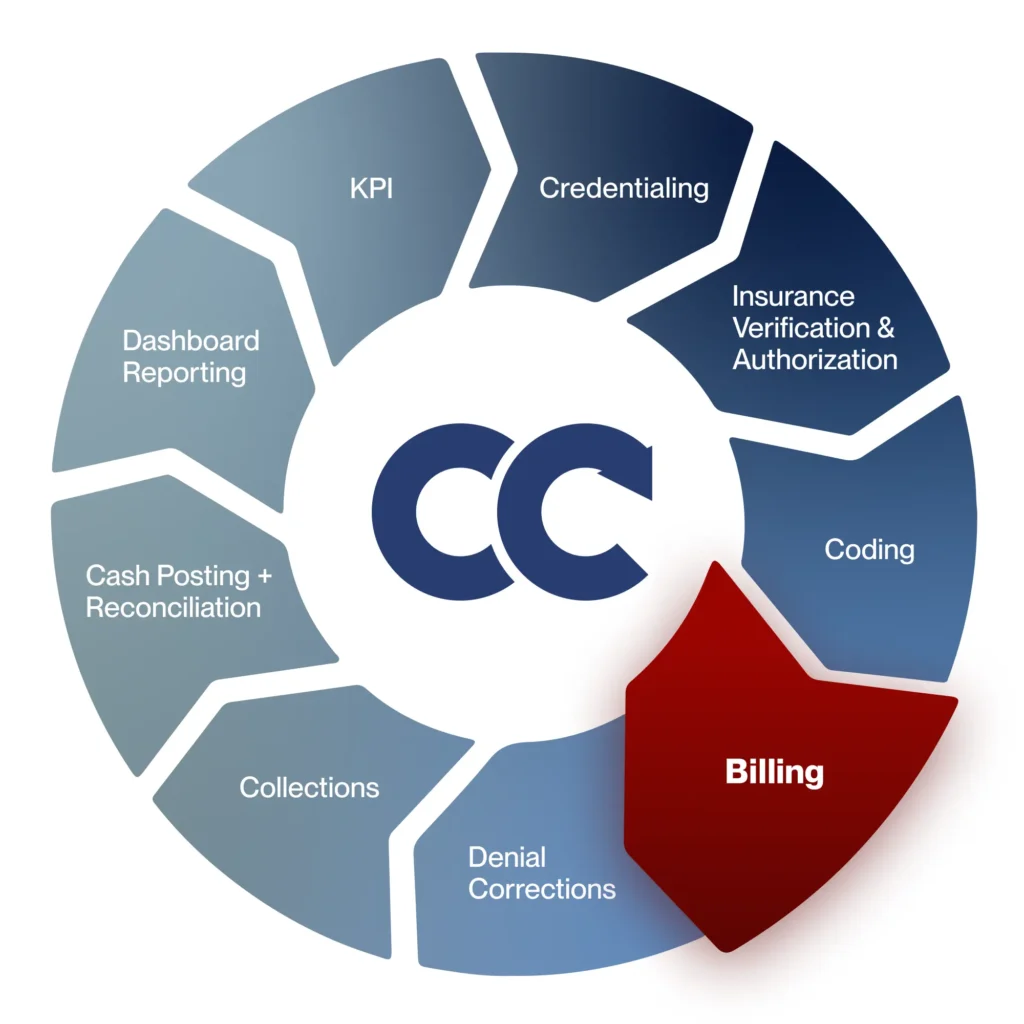
Medical billing outsourcing means handing over the billing tasks to a team of professionals who specialize in Revenue Cycle Management (RCM). It’s not just about filing claims—it’s about making sure every step of your revenue cycle works smoothly and efficiently.
From verifying insurance details to fixing claim denials and collecting payments, outsourcing covers it all.
Think of RCM as a journey that starts with your patient’s first interaction and ends with the final payment.
Outsourcing medical billing fits seamlessly into this journey, handling the most time-consuming and error-prone parts so you can focus on delivering exceptional care.
- Patient Registration and Insurance Verification: The process begins with ensuring all patient information is accurate and their insurance coverage is verified. Outsourced teams handle this step quickly and efficiently, setting a strong foundation for the rest of the billing process.
- Medical Coding and Claim Submission: Accurate coding is crucial to ensure claims are accepted by insurers. Professional billing teams are experts at applying the right codes and submitting clean claims on time, reducing the risk of rejections.
- Denial Management and Corrections: If a claim is denied or underpaid, the outsourcing team investigates the issue, corrects errors, and resubmits the claim promptly. This minimizes delays and ensures you get paid what you’re owed.
- Collections and Patient Billing: For any remaining balances after insurance payments, outsourced teams manage patient billing with clarity and professionalism. They follow up respectfully, ensuring payments are collected without straining patient relationships.
- Reporting and Insights: A great outsourcing partner doesn’t just handle the day-to-day—they also provide detailed reports and insights into your revenue cycle. This helps you make informed decisions and spot opportunities to improve your practice’s financial health.
How Do Collections Work in Healthcare?
Collections in the healthcare industry involve recovering payments for services provided to patients. This includes both payments from insurance companies and direct payments from patients.
Effective collections are a critical part of maintaining a healthcare practice’s financial health, as they ensure steady cash flow and minimize outstanding accounts receivable (A/R).
The process of collections typically includes:
- Insurance Follow-Up: Ensuring claims are processed, approved, and paid by insurers. This involves addressing any issues, such as denials or underpayments, promptly.
- Patient Billing: Communicating clearly with patients about their financial responsibility, including co-pays, deductibles, and outstanding balances.
- A/R Management: Regularly reviewing and following up on unpaid accounts to recover overdue payments while keeping the practice’s cash flow stable.
What Is the Role of Collections in the Revenue Cycle?
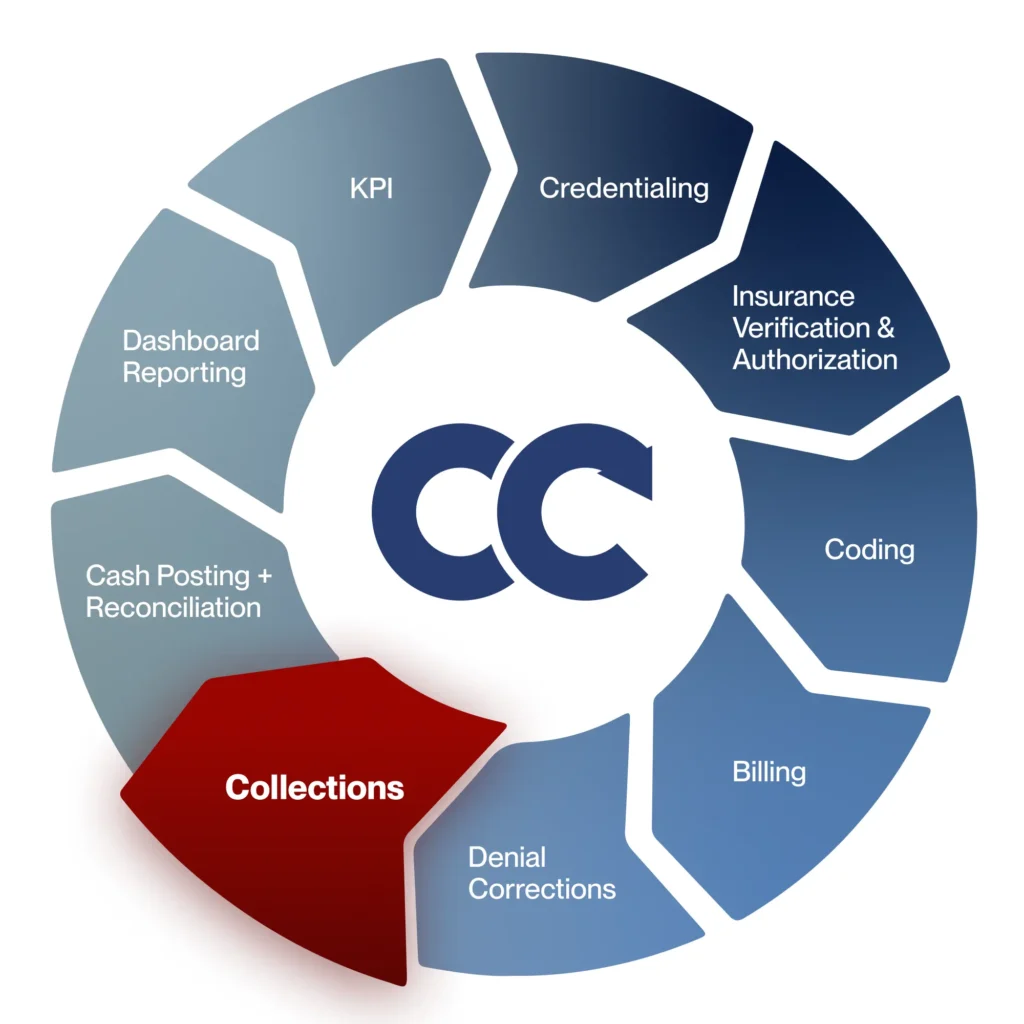
Collections are a vital phase of the revenue cycle management (RCM) process. After services are rendered and claims are submitted, the collections phase ensures that payments are received and accounts are closed.
Here’s how collections fit into the broader RCM:
- Claim Submission: Once a patient is treated, claims are submitted to insurance companies.
- Payment Posting: Insurers process claims and make payments. Patients may then receive a bill for any remaining balance.
- Collections Process: Unpaid balances are pursued, either through direct communication with the patient or follow-up with insurers.
The goal of collections is not just to recover payments but to do so in a way that maintains trust and relationships with patients.
In-House vs. Outsourced Medical Billing
When you manage medical billing in-house, everything stays under your roof. At first, this might sound like a great idea. You have direct control, can oversee every detail, and address any issues as they come up. But there’s a hidden side to it that’s often overlooked.
Handling billing in-house means hiring and training staff who are experts in medical billing and coding, which can be time-consuming and expensive. And let’s face it—staff turnover happens.
When it does, it disrupts the whole process, causing delays, errors, and added stress for everyone. On top of that, staying up-to-date with constantly changing healthcare regulations is a full-time job in itself, and one mistake could cost your practice dearly.
Now, let’s talk about outsourcing medical billing. Instead of juggling all that yourself, outsourcing means partnering with a team of experts who know billing inside and out. These professionals bring years of experience, the latest technology, and a deep understanding of how to make the billing process as smooth and efficient as possible.
By outsourcing, you’re not just handing off tasks—you’re gaining a partner who can reduce errors, speed up payments, and free up your team’s time to focus on what matters most: your patients. It’s about simplifying your workload and making your practice run more smoothly, all while improving cash flow and giving you peace of mind. It’s not just easier—it’s smarter.
Tips for Choosing the Right Outsourced Medical Billing Provider
If you decide to outsource, finding the right partner is essential. It’s not just about handing over your billing tasks; it’s about building a relationship with a team that understands your practice’s needs and goals.
Start by looking for a provider with experience in your specific field of healthcare. Different specialties have unique billing requirements, so partnering with a team familiar with your specialty ensures fewer errors and faster payments.
Transparency is another key factor. A good billing partner should provide clear, detailed reports and keep you updated on the status of claims and payments.
You should always know where your revenue cycle stands without needing to chase down information. Also, consider their use of technology.
Providers that use advanced billing software and automation tools are more likely to process claims efficiently and catch errors before submission.
Finally, don’t underestimate the importance of customer service. Your billing partner will interact with your patients regarding payments, so their approach should align with your values. Look for a team that communicates with empathy and professionalism, ensuring your patients feel respected throughout the process.
Is Outsourcing Right for Your Practice?
Every healthcare practice is unique, and whether outsourcing is right for you depends on your needs.
If you’re spending too much time on billing, struggling with claim rejections, or finding it hard to keep up with regulatory changes, outsourcing could be the solution you’ve been looking for.
Outsourcing is about more than efficiency—it’s about peace of mind. You’ll know that experienced professionals are managing your revenue cycle with care and precision, giving you the freedom to focus on what you do best: providing outstanding care for your patients.
When you think about it this way, outsourcing isn’t just a decision—it’s an investment in the health and growth of your practice.
Why Choose Cadence Collaborative?
When you partner with us, you’re not just hiring a billing and collections service—you’re gaining a dedicated team committed to your success.
Our goal is to make your revenue cycle seamless and efficient, so you can focus on providing the best care possible.
We know the healthcare industry inside and out, and we bring both expertise and a human touch to every interaction.
Our Services
At Cadence Collaborative, we manage all aspects of billing. This includes submitting claims to insurance companies, following up on unpaid claims, and ensuring payments are posted correctly. Our team works to reduce the number of denied claims and ensure you get paid as quickly as possible.
We use advanced data analytics to give you insights into your billing processes. This helps you understand where your money comes from and where issues might arise. By analyzing this data, we can help you make better decisions and improve your overall financial performance.
We work with you to find and fix any inefficiencies in your billing process. This might mean changing how things are done to save time and reduce errors. We aim to make your operations run as smoothly and efficiently as possible.
Staying compliant with healthcare regulations is crucial. We provide detailed reports and ensure that all billing processes meet regulatory standards. This keeps you informed and helps avoid any compliance issues.
Our Process
Our process ensures a seamless transition to outsourced billing and collections, providing ongoing support and optimization to maintain efficiency and compliance.
Initial Consultation
We start with an initial consultation to understand your current billing practices and identify areas for improvement. This helps us create a customized plan that meets your needs.
Implementation
Once we have a plan, we work with your staff to implement it. We provide training and support to ensure a smooth transition and minimal disruption to your operations.
Ongoing Support and Optimization
After implementation, we continue to monitor your billing and collections processes and adjust as needed to ensure they run smoothly and efficiently.
Frequently Asked Questions
How can outsourcing improve my practice’s revenue?
Outsourcing improves revenue by reducing claim denials, submitting accurate claims faster, and managing collections efficiently. Billing professionals also follow up with insurers and patients, ensuring payments are not delayed or missed. This streamlined process helps maintain steady cash flow and financial health.
Will I lose control of my billing if I outsource?
No, outsourcing doesn’t mean losing control. A reputable billing partner will provide you with regular updates, detailed reports, and full transparency throughout the process. You remain in control of your practice while benefiting from expert support and insights into your revenue cycle.
Is outsourcing medical billing secure?
Yes, reputable medical billing companies follow strict data security protocols to ensure your patient information is safe. They comply with HIPAA regulations and use secure systems to protect sensitive data from breaches or unauthorized access.
Can I outsource part of my billing instead of the entire process?
Yes, many billing companies offer flexible services, allowing you to outsource specific tasks like coding, claim submissions, or collections while keeping other functions in-house.
At Cadence Collaborative, we understand that every healthcare practice is unique, and a one-size-fits-all approach doesn’t always work. That’s why we offer flexible outsourcing solutions that allow you to customize our services to meet your specific needs.
Does outsourcing work for small practices?
Yes, outsourcing can be highly beneficial for small practices. It eliminates the need to hire and train in-house billing staff, reduces administrative burdens, and improves cash flow—allowing smaller teams to focus more on patient care.
How can I monitor my billing when it’s outsourced?
Sure thing! At Cadence Collaborative, we take pride in offering full transparency and keeping you informed every step of the way. Our dashboards are designed to give you a clear and detailed view of your revenue cycle, empowering you to make informed decisions for your practice.
In addition to dashboards, we deliver regular, comprehensive reports tailored to your needs. Whether it’s tracking key performance indicators (KPIs), understanding denial trends, or gaining insights into cash flow, we ensure you have the data you need to stay in control.
Ready to Transform Your Healthcare Operations?
Take the first step towards optimizing your agency’s performance by partnering with Cadence Collaborative. Contact us today to set up your first consultation and receive your FREE Revenue Cycle Assessment.
Call us now (401-743-2428), and let’s begin this journey toward excellence in healthcare operations.