Accurate CPT coding is the cornerstone of effective medical billing. Within urology, cystoscopy procedures are among the most frequently performed, and their coding presents unique challenges. Cystoscopy is used both diagnostically and therapeutically, which means coding errors can have significant financial and compliance consequences. For billing experts, getting cystoscopy coding right is critical, not just for reimbursement, but also for regulatory compliance and revenue integrity.
This guide explores cystoscopy CPT codes in detail, outlines common pitfalls, and provides strategies for maximizing reimbursement while staying compliant. With Cadence Collaborative’s expertise in revenue cycle management (RCM), billing professionals can rely on proven solutions to strengthen their processes and outcomes.
Understanding Cystoscopy CPT Codes
What is cystoscopy?
Cystoscopy is a minimally invasive procedure in which a urologist inserts a cystoscope, a thin, lighted tube, through the urethra to examine the bladder and lower urinary tract. This procedure helps diagnose conditions such as hematuria (blood in urine), recurrent urinary tract infections, and bladder cancer. It is also used for therapeutic interventions, including tumor removal, biopsy, and stent placement.
The cystoscope may be flexible or rigid, depending on the clinical need. Flexible cystoscopes are more commonly used for diagnostic procedures in outpatient settings, while rigid cystoscopes are often used for therapeutic interventions in hospital or surgical settings. The complexity of the equipment and the procedure itself underscores the importance of accurate coding.
Why CPT codes matter in cystoscopy billing
CPT (Current Procedural Terminology) codes are the universal language of healthcare billing. They document what procedure was performed, guide payers in determining reimbursement, and protect providers from compliance risks. In cystoscopy, accurate CPT coding is vital because:
- Reimbursement depends on it: Payers rely on CPT codes to determine appropriate payment.
- Compliance is at stake: Incorrect coding can trigger audits, penalties, or allegations of fraud.
- Revenue integrity suffers: Underbilling leads to lost income, while overbilling risks clawbacks and reputational damage.
Without accurate CPT code assignment, providers risk a cycle of denials, appeals, and delayed revenue collection. Over time, these inefficiencies can severely strain the revenue cycle and disrupt practice operations.
Common Cystoscopy CPT Codes and Their Uses
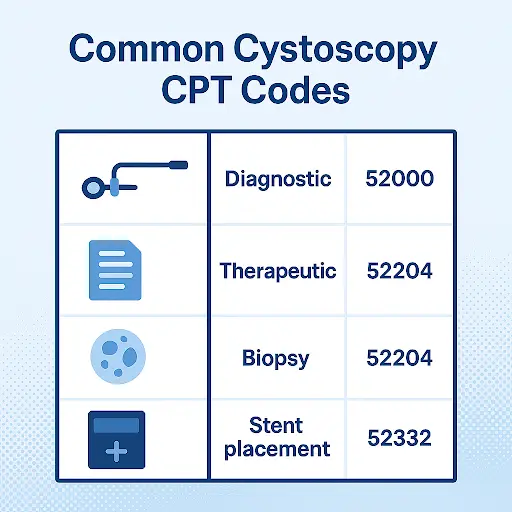
Diagnostic cystoscopy codes
The most common diagnostic cystoscopy CPT code is 52000 – Cystourethroscopy, diagnostic. This code applies when the procedure is performed solely to examine the urinary tract without intervention. Documentation should reflect that the cystoscopy was strictly diagnostic.
Diagnostic cystoscopy is typically performed for evaluation of hematuria, bladder pain, recurrent urinary tract infections, or suspected malignancy, consistent with American Urological Association (AUA) guidelines. Coders must ensure that no therapeutic intervention occurred; otherwise, the claim risks undercoding. Billing diagnostic codes correctly is essential, especially since payers often scrutinize medical necessity for these procedures.
Therapeutic cystoscopy codes
When a cystoscopy includes treatment or intervention, a different code must be applied. Examples include:
- 52204 – Cystoscopy with biopsy.
- 52214 – Cystoscopy with fulguration (minor lesion).
- 52224 – Cystoscopy with fulguration (extensive lesion).
- 52332 – Cystoscopy with ureteral stent insertion.
These codes carry higher reimbursement due to the additional complexity and resources involved. Billing specialists must confirm documentation supports therapeutic action, including details such as lesion size, location, and whether multiple interventions were performed. Missing these details in documentation can result in lost revenue opportunities.
Bundled vs. separate procedure codes
Bundling rules can complicate cystoscopy billing. Under Medicare and most commercial payer policies, if a diagnostic cystoscopy leads to a therapeutic intervention during the same encounter, only the therapeutic code should be reported. However, practices should confirm payer-specific bundling policies, as exceptions may apply. Billing both separately would constitute overbilling. On the other hand, missing the bundling rules may lead to underbilling and lost revenue.
Coders must also consider global surgical packages, where certain follow-up services may be included in the primary procedure. Failing to apply bundling rules appropriately not only impacts revenue but also exposes providers to compliance scrutiny.
Modifiers in cystoscopy billing
Modifiers provide additional context to payers. In cystoscopy billing, common modifiers include:
- 26 – Professional component only.
- 50 – Bilateral procedure.
- 52 – Reduced services.
- 59 – Distinct procedural service.
Correct use of modifiers ensures accurate claim submission, prevents denials, and reflects the full scope of the services provided. For example, modifier 50 should be applied when a procedure is performed on both ureters, but payers may have different rules on whether the service is reimbursed at 100% or 150% of the allowable amount. Understanding these nuances is essential.
Billing Challenges with Cystoscopy CPT Codes
Frequent coding errors
The most frequent mistakes include:
- Reporting diagnostic codes instead of therapeutic codes (or vice versa).
- Omitting required modifiers.
- Misinterpreting bundling rules.
Each of these errors increases denial risk and disrupts cash flow. For example, using 52000 when a biopsy was performed can lead to significant underbilling. Conversely, billing for both a diagnostic and therapeutic procedure inappropriately may trigger payer audits.
Denials and payer variations
Different payers apply different rules to cystoscopy reimbursement. For example, one insurer may bundle diagnostic and therapeutic codes, while another requires separate reporting. Some payers demand operative note details, such as lesion size or biopsy count, before approving claims. Billing teams must stay informed of these variations and tailor claims accordingly.
Failing to account for these differences often leads to claim denials, which require time-consuming appeals and rework. The cumulative effect can erode revenue and staff productivity.
Documentation gaps
Accurate coding depends on comprehensive physician documentation. Missing or vague operative notes, such as failing to specify whether a cystoscopy was diagnostic or therapeutic, can lead to downcoding or denial. Billing experts should work closely with providers to ensure that operative notes include:
- Clinical indication for the procedure.
- Type of cystoscopy performed.
- Lesion size, number, and location.
- Interventions performed.
- Laterality (if applicable).
Coders should also educate providers on how small details impact reimbursement. For example, specifying that fulguration involved “extensive lesions” may shift coding from 52214 to 52224, which carries higher reimbursement.
Best Practices for Accurate Cystoscopy Billing
Stay updated with CPT coding changes
CPT codes and payer rules change annually. A code valid this year may be obsolete the next. Billing teams should:
- Subscribe to AMA and CMS updates.
- Participate in ongoing coding education.
- Update EHR systems promptly with new codes.
Failure to stay updated can result in non-compliant claims and delayed reimbursement. Even a single outdated code can cascade into repeated denials and lost revenue.
Ensure thorough documentation
Billing accuracy begins with clinical documentation. Physicians should document medical necessity clearly and tie it directly to the CPT code used. For example, a cystoscopy with biopsy should note the lesion observed, its clinical significance, and the action taken. Clear documentation not only supports coding accuracy but also strengthens appeals in case of denials and helps practices defend against payer audits or compliance reviews.
Leverage technology and audits
EHRs and coding software can support accurate CPT selection and alert teams to missing modifiers. In addition, routine internal and external audits catch errors early and provide insights into payer-specific denial patterns. These proactive steps save time, reduce denials, and protect compliance.
Audits can also identify trends, such as consistently undercoding certain therapeutic cystoscopies. Identifying these patterns allows practices to correct errors and recover revenue that may otherwise go unnoticed.
Partnering with experts like Cadence Collaborative
For many practices, cystoscopy coding complexity exceeds internal capacity. Outsourcing to Cadence Collaborative provides:
- Access to coding experts with deep urology knowledge.
- Streamlined workflows that reduce administrative burden.
- Denial management strategies that recover lost revenue.
- Compliance assurance to safeguard against payer audits.
By partnering with a trusted RCM firm, providers can focus on patient care while improving financial performance. Expert support is particularly valuable in specialties like urology, where coding errors can easily escalate into significant compliance risks.
Maximizing Reimbursement and Compliance
Appeals and denial management strategies
Denied cystoscopy claims can be recovered with a strong appeal strategy. Successful appeals include:
- Attaching operative notes with full details.
- Citing payer-specific policy language.
- Demonstrating medical necessity.
Billing teams should develop workflows for quick identification and appeal of denials, reducing write-offs, and improving cash flow. Practices with formal denial management programs consistently recover more revenue than those without.
Compliance with CMS and payer guidelines
Cystoscopy billing must align with CMS and private payer regulations. Overbilling can be flagged as fraud or abuse, while underbilling undermines revenue. Practices should:
- Train staff in compliance policies.
- Maintain updated coding manuals.
- Use compliance audits to identify and mitigate risk.
Beyond compliance, proactive adherence to guidelines builds payer trust and reduces audit risk. A reputation for accuracy can lead to smoother claim processing and faster payments.
Future trends in urology billing
The future of cystoscopy billing will be shaped by technology. Artificial intelligence (AI) and machine learning tools are emerging to:
- Automate code selection.
- Flag documentation gaps.
- Predict payer denials based on historical data.
As automation expands, billing teams will need to blend AI tools with expert oversight to ensure accuracy and compliance. Practices adopting these technologies early will benefit from reduced errors, improved efficiency, and greater revenue capture.
Another trend is increased payer scrutiny. Rising healthcare costs and regulatory initiatives, such as CMS’s Program Integrity efforts, have prompted payers to tighten claim review processes, increasing the importance of precise coding and robust documentation.. Billing teams must anticipate this trend by ensuring impeccable documentation and coding accuracy.
Additional Tips for Billing Experts
- Coordinate with clinical staff: Regular communication between coders and physicians reduces documentation errors.
- Develop payer-specific cheat sheets: Summarize unique requirements for major payers to speed up claim submission.
- Monitor key metrics: Track denial rates, days in accounts receivable, and coding accuracy to measure performance.
- Educate continuously: Regular workshops and training ensure staff remain updated on best practices.
Conclusion
Accurate cystoscopy CPT coding is not optional; it is essential. From diagnostic cystoscopies to complex therapeutic interventions, coding errors can undermine reimbursement, trigger denials, and create compliance risks. Billing professionals must stay informed of coding updates, understand bundling and modifier rules, and ensure thorough documentation.
Cadence Collaborative specializes in guiding healthcare providers through these challenges. With expertise in urology billing, our team delivers solutions that protect compliance, improve reimbursement, and strengthen overall revenue cycle performance.
For providers seeking to eliminate coding errors and maximize revenue, partnering with Cadence Collaborative is the next step.
Contact us today to learn how our specialized billing and coding support can streamline your urology practice and secure compliance in every claim.