Have you ever had a claim denied because the diagnosis didn’t seem to “match” the procedure? If so, you’re not alone. One of the most misunderstood, yet absolutely critical elements of medical billing is the diagnosis pointer. Misusing this small detail can derail claims, frustrate providers, and stall revenue.
In today’s highly regulated healthcare environment, revenue cycle management depends on precision. Even minor documentation issues, such as misusing a diagnosis code pointer, can create major problems. Billing accuracy isn’t just about keeping payers happy; it directly affects compliance, efficiency, and the financial health of your organization.
By the end of this article, you’ll know exactly how to use diagnosis pointers correctly to improve medical billing accuracy, reduce denials, and strengthen your practice’s revenue cycle.
What is a Diagnosis Pointer in Medical Billing?
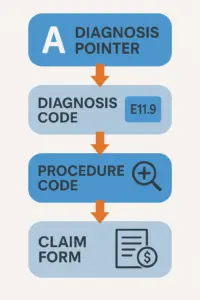
A diagnosis pointer is a small but powerful element of a claim. It’s not the diagnosis itself — it’s the link that connects a diagnosis to the specific service or procedure performed.
- Diagnosis codes (ICD-10 coding) describe a patient’s condition.
- Pointers indicate which diagnosis applies to each procedure listed on a claim.
Example: A pointer “A” might represent diabetes (ICD-10: E11.9), and that pointer is linked to a lab test for HbA1c. Without this link, the payer may not see the medical necessity of the test.
The distinction between a diagnosis and a diagnosis code pointer is critical: the diagnosis code identifies the patient’s condition, while the pointer justifies the clinical rationale for the service rendered.
Why Diagnosis Pointers Matter for Accurate Billing
Diagnosis pointers serve one essential purpose: proving medical necessity. Insurance companies want to ensure that the patient’s documented diagnoses justify procedures. Without a clear linkage, claims can be flagged, delayed, or denied.
- Improper use can lead to claim denials, delayed claim reimbursement, or even compliance issues.
- Accurate use ensures faster payments, fewer rejections, and reduced administrative burden.
Although often overlooked, diagnosis pointers are essential safeguards for revenue integrity. They support audit readiness, reduce manual rework, and demonstrate a provider’s commitment to accuracy. In other words, the effective use of a diagnosis pointer is just as important as the ICD-10 code itself.
How Diagnosis Pointers Work in Claims
On the CMS-1500 claim form, each CPT (procedure) code can be linked to one or more diagnosis pointers.
- A procedure may reference a single pointer (A) or multiple pointers (A and B) if more than one condition supports the service.
- Each pointer corresponds to the diagnosis code listed in Box 21.
Example:
- CPT: 83036 (HbA1c test) → Pointer “A” (diabetes, E11.9)
- CPT: 99213 (office visit) → Pointers “A” and “B” (diabetes and hypertension)
This direct linking shows payers the medical logic behind each billed service. When the diagnosis code pointer is accurately applied, it eliminates ambiguity and accelerates claim reimbursement.
Common Errors with Diagnosis Pointers (and How to Avoid Them)
Errors with pointers can cause unnecessary denials and create compliance risks. Common mistakes include:
- Using the wrong diagnosis link – mismatching the service and condition.
- Omitting secondary conditions – failing to list additional diagnoses that justify the procedure.
- Overusing pointers – assigning every diagnosis to every procedure, which confuses payers and weakens the claim.
Example: Linking a “routine exam” diagnosis to a surgical procedure creates a mismatch that almost guarantees denial.
Each of these errors affects medical billing accuracy. Left unchecked, they can escalate into larger problems such as increased accounts receivable, compliance findings, or strained payer relationships. Providers who implement strong review processes around diagnosis pointer usage can avoid these pitfalls.
Best Practices for Using Diagnosis Pointers Correctly
Improving your use of diagnosis pointers requires attention to detail and proactive management. To strengthen medical billing accuracy:
- Always link the most relevant diagnosis to the procedure performed.
- Stay updated with payer-specific rules (Medicare, Medicaid, and commercial carriers).
- Use coding software or conduct regular expert reviews to prevent mismatches.
- Implement a diagnosis pointer checklist for your billing team to ensure consistency and compliance.
Prioritize Staff Training and Audits
Ongoing staff education and periodic coding audits are critical. Teams must understand not only how pointers work but also why they matter. By investing in continuous training and compliance reviews, practices can reduce errors, adapt to payer-specific requirements, and protect long-term revenue performance.
Training should specifically connect ICD-10 coding to claim accuracy. Staff who understand the relationship between diagnosis codes, pointers, and reimbursement are better equipped to deliver cleaner claims and improve first-pass acceptance rates.
Incorporating Technology
Advanced practice management systems and automation tools can systematically detect mismatches between CPT codes and diagnosis pointers, reducing manual oversight and improving claim accuracy. These technologies act as guardrails, ensuring that services are always paired with the correct diagnoses. However, human oversight is still essential, as payers often update their rules.
Real-World Example of Diagnosis Pointer Use
Imagine a patient with diabetes (E11.9) and hypertension (I10):
- HbA1c lab test → Pointer “A” (diabetes)
- Blood pressure evaluation → Pointer “B” (hypertension)
This clarity ensures that the payer understands why both services were provided, resulting in faster claim reimbursement and fewer denials.
Another example: A patient presents with chronic kidney disease (N18.9) and anemia (D64.9). A lab test for hemoglobin is ordered. Linking the correct pointer ensures that the payer recognizes the anemia diagnosis as the justification for the lab, while the kidney disease is documented but not incorrectly tied to unrelated services.
These examples highlight why effective use of a diagnosis code pointer is essential for both compliance and financial performance.
The Financial Impact of Diagnosis Pointers
It’s easy to underestimate the financial importance of these small claim details. But for a practice submitting thousands of claims monthly, pointer errors can add up to significant revenue loss. Delayed or denied claims increase rework costs, staff frustration, and payer friction.
Correct use of a diagnosis pointer streamlines revenue cycle performance:
- Reduced denials = more predictable cash flow.
- Fewer appeals = lower administrative costs.
- Accurate documentation = stronger compliance posture.
In healthcare finance, small details have large consequences. Ensuring medical billing accuracy through proper pointer use is a low-cost, high-value strategy.
How Diagnosis Pointers Fit into Revenue Cycle Management
At Cadence Collaborative, we know that errors in diagnosis code pointers can cause ripple effects throughout the entire revenue cycle:
- Mistakes at the front end (eligibility, intake, coding) can delay payment and increase accounts receivable.
- Incorrect or incomplete diagnosis pointers can lead to cascading denials, slowing cash flow.
- Proper pointer use reduces denials, improves compliance, and accelerates claim reimbursement.
Cadence Collaborative applies a proactive, end-to-end approach to revenue cycle management, ensuring diagnostic accuracy, compliance, and optimized reimbursement at every stage of the billing cycle. By integrating robust training, advanced technology, and expert oversight, we prevent errors with diagnosis pointers that might otherwise result in compliance risks and costly revenue leakage.
Our goal is not just to submit claims, but to help providers build a sustainable financial model. By focusing on ICD-10 coding, compliance, and billing efficiency, we provide the tools practices need to thrive.
Conclusion
Diagnosis pointers may be small codes, but they have a big financial impact. Correct use can mean the difference between smooth reimbursement and frustrating denials. When applied correctly, they serve as the bridge between clinical documentation and financial performance.
Now is the time to review your claims process and spot gaps in how your team handles pointers. Even incremental refinements in diagnosis pointer usage can materially reduce errors, reinforce compliance, and yield measurable improvements in financial performance.
Contact Cadence Collaborative at (401) 743-2428 to streamline your billing process, reduce denials, and accelerate reimbursements. With deep expertise in ICD-10 coding, diagnosis pointers, and revenue cycle management, we help providers improve efficiency and achieve financial stability.