At Cadence Collaborative, we know that credentialing is more than just paperwork—it’s the essential first step in creating a strong and efficient revenue cycle.
Credentialing isn’t just a box to check; it’s the foundation of trust and transparency between healthcare providers, insurance companies, and patients.
Let’s explore what credentialing is, why it matters, and how to get it right, every time.
What Is Credentialing?
Credentialing is the process of verifying a healthcare provider’s qualifications, training, and experience to ensure they meet the standards required by insurance networks and regulatory bodies.
It’s a formal handshake between providers and payers, confirming that the services offered meet professional and ethical standards.
Think of credentialing as your practice’s ticket to accessing patients through insurance plans. Without it, even the most skilled providers can find themselves out of network—and out of reach for patients.
Why Is Credentialing the First Step in Revenue Cycle Management (RCM)?
Credentialing sets the tone for everything that follows in the revenue cycle. If it’s not done properly, it can lead to claim denials, revenue loss, and frustration for both providers and patients. Here’s why it’s so important:
- Streamlines Insurance Reimbursement: Credentialed providers are recognized by payers, ensuring claims are processed smoothly and promptly.
- Builds Patient Trust: Patients feel confident knowing their provider is vetted and accepted by their insurance.
- Reduces Claim Denials: Accurate credentialing eliminates common errors that can lead to denied claims.
- Supports Regulatory Compliance: Credentialing ensures your practice adheres to state and federal healthcare regulations.
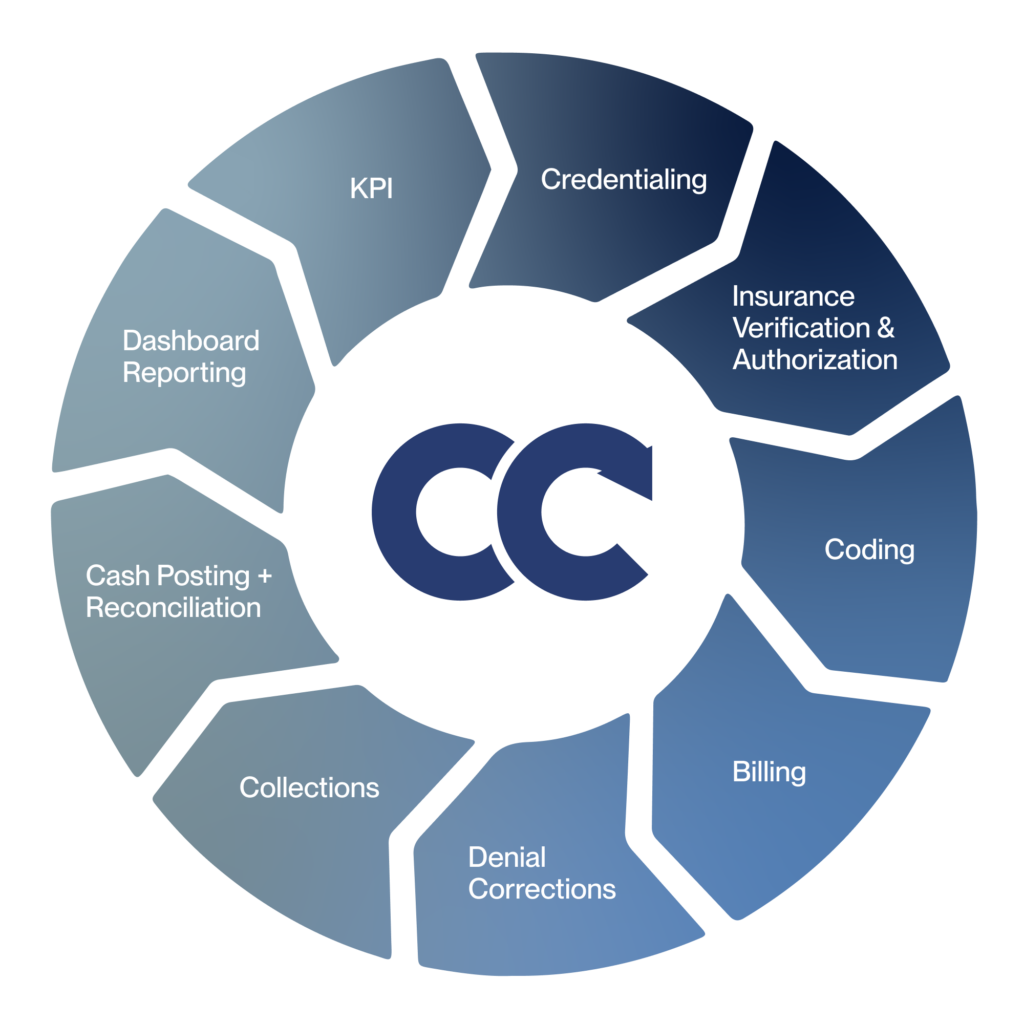
At Cadence Collaborative, we treat credentialing as the keystone of RCM, ensuring your practice is set up for success from the very beginning.
The Credentialing Process: How It Works
Credentialing can seem complex, but it boils down to a few key steps:
- Gathering Provider Information: This includes licenses, certifications, education history, work experience, malpractice insurance, and references.
- Submitting Applications: Applications are submitted to insurance networks, government programs like Medicare and Medicaid, or hospitals.
- Verification: Payers conduct primary source verification to confirm the accuracy of the provider’s credentials.
- Approval: Once credentials are verified, the provider is officially added to the network, making their services reimbursable.
Each payer may have slightly different requirements and timelines, which is why having an experienced partner like Cadence Collaborative can make all the difference.
Common Challenges in Credentialing—and How to Overcome Them
While credentialing is essential, it’s not without its challenges. Here are some hurdles we frequently see and how we help practices overcome them:
- Incomplete Applications: Missing documents or outdated information can delay the process. We conduct thorough reviews to ensure every application is accurate and complete.
- Lengthy Timelines: Credentialing can take weeks or even months. We leverage our expertise and payer relationships to expedite the process wherever possible.
- Lack of Resources: Smaller practices often struggle to allocate time and staff to credentialing. Our team acts as an extension of your practice, handling the details so you can focus on patient care.
- Re-Credentialing Deadlines: Providers must renew their credentials periodically. We track these deadlines and proactively manage renewals to keep you compliant.
Credentialing vs. Privileging: Understanding the Difference
It’s common to hear credentialing and privileging mentioned together, but they’re distinct processes.
Credentialing verifies a provider’s qualifications, ensuring they meet the standards required to practice medicine and participate in insurance networks.
Privileging, on the other hand, is about granting specific permissions within a healthcare facility, such as the ability to perform surgeries or use specialized equipment.
While they often occur simultaneously, credentialing is the broader process that sets the stage for privileging to take place.
Credentialing for Group Practices vs. Individual Providers
Credentialing a group practice comes with unique complexities.
Each provider within the group must be individually credentialed while also aligning with the practice’s overarching insurance contracts. This dual-layered approach requires meticulous organization and oversight.
For individual providers, the process is more straightforward but equally critical, as missing credentials can mean delayed reimbursements or exclusion from key payer networks.
Our expertise ensures that both group practices and individual providers achieve seamless credentialing.
Re-Credentialing: Staying Ahead of the Curve
Credentialing isn’t a one-and-done task. Providers must renew their credentials periodically to stay in network and maintain compliance.
Re-credentialing involves updating documentation, verifying continued compliance with standards, and addressing any changes in provider status.
Practices that neglect re-credentialing risk interruptions in reimbursements and patient dissatisfaction.
How Cadence Collaborative Simplifies Credentialing
At Cadence Collaborative, we understand that credentialing can feel like a daunting and time-consuming process. That’s why we’ve developed a seamless approach to make it easier for healthcare providers and practices.
Our deep expertise in navigating payer requirements means we know exactly what it takes to get your applications right on the first try.
By handling the complexities of credentialing with precision, we save you valuable time and reduce the risk of delays.
Our support doesn’t stop at submitting applications. We take care of every detail, from collecting the necessary documentation to ensuring that all payer communications are managed efficiently.
With our end-to-end services, you can trust us to stay on top of every step in the process, so you never have to worry about missing deadlines or dealing with follow-ups.
We also tailor our credentialing solutions to meet the unique needs of your practice. Whether you’re a small clinic or a larger organization, we adapt our approach to fit your workflows and priorities.
By acting as an extension of your team, we allow you to focus on patient care while we handle the administrative burdens.
FAQs About Credentialing
How long does the credentialing process take?
On average, credentialing takes 60-90 days, but timelines can vary based on payer response times. Working with Cadence Collaborative can help streamline the process.
What happens if a provider isn’t credentialed?
Without credentialing, claims may be denied, and patients may be unable to use their insurance. This can result in revenue loss and frustrated patients.
Can Cadence Collaborative handle re-credentialing?
Absolutely. We manage re-credentialing deadlines and ensure all renewals are completed on time to avoid lapses in network participation.
Is credentialing required for all providers?
Yes, any provider seeking reimbursement from insurance companies or government programs must be credentialed.
What information is needed for credentialing?
Typical requirements include licenses, certifications, education history, malpractice insurance, work experience, and references.
Build Your Practice’s Future with Confidence
Credentialing may seem like a behind-the-scenes process, but its impact is felt everywhere—from smoother patient experiences to a healthier bottom line.
At Cadence Collaborative, we don’t just help you meet the requirements; we position your practice for long-term success.
By handling credentialing with expertise and care, we allow you to focus on what you do best: delivering exceptional care to your patients.
Ready to take the first step? Let’s get started together. Contact us today!






