Billing for mental health services shouldn’t feel like a second job. But let’s be real—it often does.
If you’re a therapist, psychologist, or psychiatrist, chances are you got into this field to help people, not to drown in insurance claims, CPT codes, and denied reimbursements.
Yet, here you are, chasing payments instead of focusing on what truly matters: your patients.
The reality? Mental health billing is different.
Unlike general medical billing, it comes with extra layers of complexity—session limits, authorization headaches, and insurance policies that seem to change overnight.
And if your billing isn’t dialed in, your cash flow suffers.
But here’s the good news: you don’t have to do it alone. With the right approach (and the right billing solutions), you can cut through the red tape, get paid faster, and spend more time doing what you do best—helping people.
In this guide, we’re breaking down:
- Why mental health billing is such a nightmare (and how to fix it)
- The best ways to avoid insurance denials and delayed payments
- How to streamline your billing without sacrificing patient care
Let’s get into it.
Why Is Mental Health Billing So Complex?
If you’ve ever felt like mental health billing is way harder than it should be, you’re not wrong.
Unlike standard medical billing, where a procedure is a procedure and a diagnosis is a diagnosis, mental health services operate in a world of gray areas, shifting policies, and endless insurance loopholes.
1. Session Limits and Authorization Hassles
Imagine this: You have a patient who needs weekly therapy. They’re making progress.
Then suddenly, their insurance decides they’ll only cover eight sessions per year—because, apparently, mental health has a limit? (Spoiler: It doesn’t.)
Navigating pre-authorizations and session caps is one of the biggest challenges in mental health billing.
Insurance companies often require extra paperwork or proof of “medical necessity,” making you jump through hoops just to get paid for care that should be standard.
2. Complicated CPT Codes and Reimbursement Rules
Not all therapy sessions are created equal—at least in the eyes of insurance. Did you bill for a 45-minute session or 60? Was it individual or family therapy? In-person or telehealth?
Every detail affects how (and if) you get reimbursed. If you use the wrong CPT code or miss a minor documentation requirement, expect delays, denials, and endless resubmissions.
3. Insurance Companies Playing Hard to Get
Ever sent a clean, perfectly coded claim only to have it rejected with zero explanation? Yeah, you’re not alone.
Insurance companies deny claims for the smallest reasons—or no clear reason at all. Sometimes it’s a coding error.
Other times, it’s just bureaucracy in action. And when you do get paid? Reimbursement rates for mental health services are often lower than other medical fields, making it even more frustrating.
4. Telehealth
Teletherapy has revolutionized mental health care, but insurance companies are still playing catch-up. Some cover virtual sessions like in-person visits. Others don’t. Some require special modifiers. Others demand proof that therapy over Zoom is just as effective (again—spoiler: It is).
All of this uncertainty makes billing for telehealth services a moving target. And when policies change without warning, keeping up feels impossible.
So, What’s the Solution?
It starts with having the right billing strategies and tools in place—because winging it and hoping for the best isn’t a business plan.
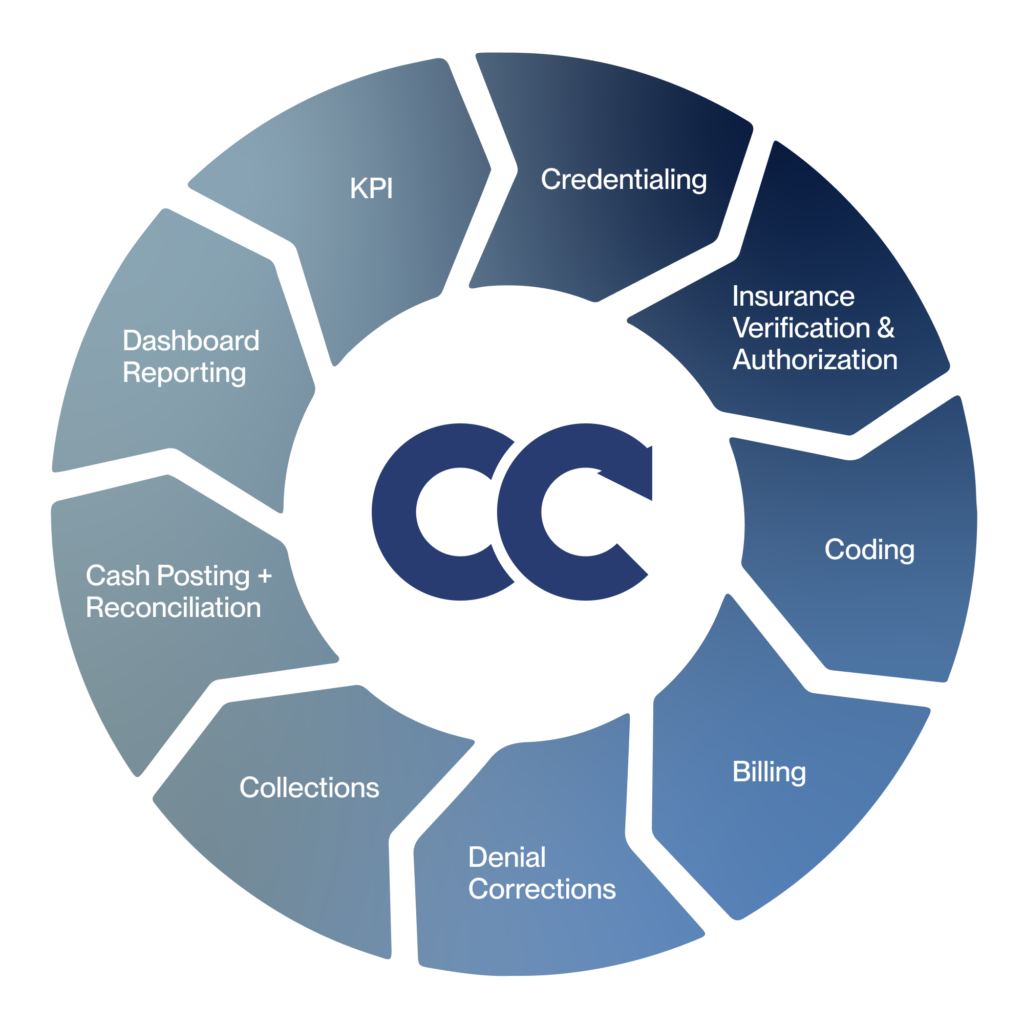
This is where Cadence Collaborative comes in. If billing has become a never-ending headache, we help mental health professionals take back control—without drowning in paperwork.
From insurance verification to claims management and denial prevention, our solutions are designed to simplify the billing process and maximize reimbursements.
Because at the end of the day, you should be focused on patient care—not chasing down insurance payments.
How to Simplify Mental Health Billing
Alright, let’s get into the actionable fixes. Here’s how to cut through the complexity and start getting paid on time, every time.
1. Verify Insurance Benefits Upfront
Ever had a session with a new client, only to find out later their insurance won’t cover it? Now you’re stuck in the awkward position of chasing payments—or worse, writing it off.
The fix? Always verify insurance benefits before the first session. This means:
- Checking if pre-authorization is required
- Confirming session limits and coverage details
- Understanding copays and deductibles before treatment starts
If this sounds like a hassle, we can handle it for you.
Our insurance verification services prevent surprises—so you don’t waste time on denied claims or unexpected out-of-pocket costs for patients.
2. Bill Smarter, Not Harder (Get Your Codes Right the First Time)
Insurance companies love rejecting claims over tiny errors. Using the wrong CPT code, forgetting a modifier, or missing a diagnosis link? Expect delays.
To get paid faster:
- Use the correct CPT codes for session length (e.g., 90834 for 45 minutes, 90837 for 60)
- Add necessary modifiers for telehealth (e.g., “95” for virtual sessions)
- Double-check documentation before submitting—because one missing detail can mean weeks of waiting
3. Automate Everything You Can
Still manually tracking claims, sending invoices, and chasing payments? Stop. Billing software and expert revenue cycle management solutions can automate most of this process, freeing you up for patient care.
A streamlined system means:
- Claims are submitted electronically (no snail mail delays)
- Denials are flagged and fixed quickly
- Payments get processed faster, improving cash flow
The Most Common CPT Codes for Mental Health Billing
Getting the right CPT codes on your claims isn’t just about avoiding denials—it’s about getting paid what you’re worth.
Mental health billing has specific codes for different therapy types, session lengths, and services. Use the wrong code, and you risk underbilling—or worse, claim rejection.
Here are the most frequently used CPT codes for mental health providers, so you can bill correctly and maximize reimbursements.
Individual Therapy CPT Codes

These codes are used for one-on-one psychotherapy sessions and are based on session length:
- 90832 → 30-minute psychotherapy session
- 90834 → 45-minute psychotherapy session
- 90837 → 60-minute psychotherapy session (most commonly used)
Pro tip: Some insurance companies won’t reimburse 60-minute sessions (90837) at full rate, so check payer-specific policies to avoid payment reductions.
Add-On Codes for Extended Psychotherapy Sessions
For therapy sessions that include both psychotherapy and an E/M (Evaluation & Management) service, use these add-on codes in combination with standard psychotherapy codes:
- 90833 → 30-minute psychotherapy add-on for E/M visits
- 90836 → 45-minute psychotherapy add-on for E/M visits
These codes must be billed alongside an E/M service code (e.g., 99212–99215) and cannot be used as standalone psychotherapy sessions.
They are most commonly used by psychiatrists, psychiatric nurse practitioners, and other prescribers who provide both therapy and medication management.
Crisis Therapy CPT Codes
When a patient is experiencing a mental health crisis, you should bill for crisis therapy, which has higher reimbursement rates:
- 90839 → First 60 minutes of crisis psychotherapy
- +90840 → Each additional 30 minutes beyond the first hour
Family & Couples Therapy CPT Codes

If therapy includes family members or partners, these codes apply:
- 90846 → Family therapy without the patient present
- 90847 → Family therapy with the patient present
- 90849 → Multiple-family group therapy
Group Therapy CPT Codes

For therapy provided in a group setting, use these codes:
- 90853 → Standard group therapy session
- 90849 → Multiple-family group therapy (when family members participate)
Pro tip: Group therapy has lower reimbursement rates than individual sessions, but can be a great way to increase revenue while helping more clients.
Psychiatric Diagnostic Codes (First-Time Patient Evaluations)
When seeing a new patient for an initial assessment, use:
- 90791 → Psychiatric diagnostic evaluation without medical services
- 90792 → Psychiatric diagnostic evaluation with medical services (includes medication management, used by psychiatrists or prescribers)
Pro tip: 90791 is one of the highest reimbursed codes in mental health billing, but most payers only allow it once per year per patient.
Neuropsychological Testing and Cognitive Assessment
When conducting neuropsychological or cognitive assessments, providers should use:
- 96130 → First hour of psychological or neuropsychological testing evaluation (includes integration of patient data, clinical decision-making, and report preparation)
Pro tip: If additional time is needed beyond the first hour, use add-on code 96131 for each additional 30 minutes. This code is often required for ADHD, dementia, or cognitive decline assessments and must be supported by detailed documentation.
Medication Management Codes (For Prescribers)
For psychiatrists, psychiatric nurse practitioners, and other prescribing providers, medication management sessions use:
- 99212-99215 → Office visits for medication evaluation & management (E/M services)
- +90863 → Medication add-on code (used alongside therapy session codes when a provider also manages meds)
Pro tip: Insurance often requires a therapy session to be billed alongside medication management—standalone med checks may not be covered.
The Right Modifiers Can Make or Break Your Reimbursement
Ever had a clean claim denied for no apparent reason? Or got reimbursed less than expected? The culprit might be missing or incorrect modifiers.
Modifiers are two-character codes added to CPT (Current Procedural Terminology) codes that give insurance companies more details about the session—like whether it was telehealth, an extended session, or provided under special circumstances.
- Using the right modifier ensures that:
Your claim isn’t rejected for incomplete information
You receive the correct reimbursement amount
Insurance payers process your claim faster
Let’s break down the most commonly used modifiers for mental health billing.
Telehealth Modifiers
With virtual therapy sessions more common than ever, using the right modifier is essential for getting reimbursed for telehealth.
- Modifier 95 → Used for synchronous telemedicine services (live video therapy). Most commercial payers and some Medicaid plans require this.
- Modifier GT → Similar to 95, but often required for Medicare and Medicaid plans in certain states.
Pro tip: Always verify which modifier the insurance plan prefers before submitting claims—some will reject a claim if the “wrong” telehealth modifier is used.
Extended Session Modifiers
Sometimes, therapy runs longer than expected—and you should be paid for that extra time. These modifiers help ensure you get full reimbursement for extended sessions:
- Modifier +90840 → Add-on code for crisis psychotherapy beyond the first 60 minutes.
- Modifier 22 → Used when a session requires significantly more time and effort than usual (documentation must justify this).
Medicare-Specific Modifiers
If you bill Medicare for mental health services, there are unique modifiers to be aware of:
- Modifier GQ → Used for asynchronous telehealth (store-and-forward technology)—not common for therapy but required in some cases.
- Modifier KX → Used when a Medicare therapy cap has been exceeded but continued treatment is medically necessary.
Modifiers for Services Provided by Supervised Clinicians
When services are provided by a clinician under supervision, some insurance payers require specific modifiers to clarify billing details:
- Modifier AH → Used to indicate services were provided by a clinical psychologist.
- Modifier AJ → Used for services provided by a clinical social worker.
- Modifier HO → Used for masters-level therapists, including licensed professional counselors (LPCs) and marriage and family therapists (LMFTs).
Pro tip: Always check with insurance payers about who can bill under their own NPI vs. who needs a supervising provider.
Billing Issues Are Just the Tip of the Iceberg
If you think your biggest problem is insurance claims getting denied or payments taking forever, here’s the real issue: your entire revenue cycle might be working against you.
Billing is just one piece of a bigger system—Revenue Cycle Management, which controls everything from insurance verification to final reimbursement.
And when any part of that system breaks, your practice bleeds money, time, and energy.
Let’s talk about the real questions mental health providers are asking.
Why Are Insurance Payments So Slow?
You submit a claim. Weeks pass. No payment.
It’s frustrating, but it’s also predictable. Insurance companies don’t rush to pay you—and they have plenty of ways to slow things down:
- Claims get held up over missing details or coding errors.
- Delays are built into the system—some insurance plans simply take longer to process.
- Payers use stalling tactics like requesting “more documentation” (even when it’s not necessary).
A structured revenue cycle tracks every claim in real-time, flags delays, and follows up relentlessly—so your payments don’t get lost in the system.
How Can I Reduce Claim Denials?

Nothing kills cash flow faster than denied claims. And here’s the kicker: most denials are avoidable.
The most common reasons mental health claims get denied?
- Coding mistakes (especially for telehealth or extended sessions).
- Lack of prior authorization, even if you’ve worked with the patient before.
- Session limits exceeded without enough clinical justification.
Instead of fixing denials after the fact, a strong revenue cycle prevents them from happening in the first place—by ensuring clean claim submission, catching errors before they cause problems, and handling pre-authorizations proactively.
Should I Drop Insurance and Go Private Pay?
Every mental health provider asks this at some point. Insurance billing is a headache—so why not cut it out altogether?
Why some providers drop insurance:
- Fewer claim issues, less admin work.
- Faster, direct payments.
- Total control over session rates.
Why it’s not always the best move:
- Fewer patients can afford private pay.
- You lose a steady stream of insurance-covered sessions.
- You still have to track payments and outstanding balances.
Instead of choosing insurance or private pay, a well-managed revenue cycle lets you balance both.
By optimizing insurance reimbursements and automating out-of-pocket billing, you keep revenue flowing from all sides—without the stress.
Get Paid What You Deserve—Without the Billing Stress
You didn’t start your practice to chase down insurance payments, fix rejected claims, or spend your evenings drowning in billing paperwork. Your focus should be on your patients—not on fighting a broken system just to get paid.
But here’s the truth: mental health providers who take control of their revenue cycle see a massive difference.
✔ Faster reimbursements mean no more waiting months for payments.
✔ Fewer denials mean less time fixing mistakes and more time with patients.
✔ A predictable cash flow means less stress and more stability for your practice.
At Cadence Collaborative, we take the burden of billing off your plate—so you can get paid on time, every time, without the frustration.
Let’s simplify your billing process. Contact us today and see how we can help your practice thrive—without the financial headaches.